
Pivoting on a dime
COVID-19 has led many substance use disorder (SUD) treatment providers to shift to telehealth in order to deliver care. This transition has highlighted the benefits of telehealth as a tool that can broaden access to treatment beyond the pandemic. It can provide new pathways for patients, including individuals in rural communities.
The challenges of the past year have also brought barriers around internet and technology into clearer focus: In order to take advantage of telehealth, patients in rural communities may need support such as:
- Internet hotpots
- Facilities where technology is provided
- Universal Service Administrative Co.'s Lifeline program for broadband
A growing library of resources is available for rural providers implementing telehealth, including:1
- Health Resources and Services Administration telehealth website
- Rural Health Information Hub Rural Telehealth Toolkit
- For broadband/internet, Universal Service Administrative Co.’s Rural Health Care program
- Center for Connected Health Policy, which includes information about policy changes due to COVID at the federal and state levels
- Information on flexibilities during COVID-19 (Providers should remain current on federal and state policies and third-party billing considerations as they may change during and after the pandemic.)
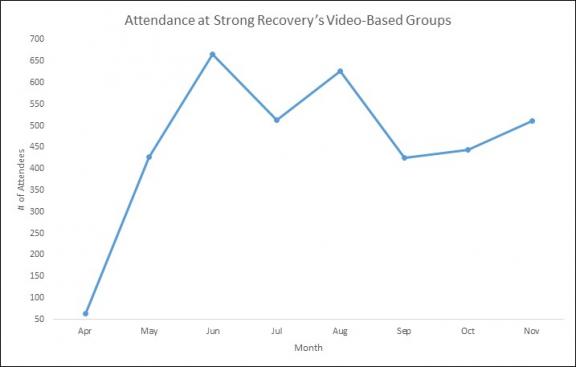
Strong Recovery in Western New York is one of the SUD treatment programs that has learned lessons about telehealth during COVID. Along with delivering individual therapy by phone and video to prevent spread of the virus, they converted their in-person group therapy to an online format over a six-week period last spring.
As Patrick Seche, senior director of addiction services, explains, the pandemic “forced us to pivot on a dime … to provide valuable services to our patients.”
In late summer, Strong Recovery was able to reinstate some in-person groups. They are now operating under a hybrid system, with most groups held online and several held in person again at their clinic.
New pathways
The program is evaluating what group therapy—a particular strength of theirs—should look like after the pandemic. They are collecting feedback from patients and staff and assessing outcomes, needs, and preferences.
Videoconferencing has opened doors for patients who find it easier to, or would rather, meet from home. In-person meetings are the best format for other patients, including those with limited access to technology. (During the pandemic, individual therapy by phone has been another option.)
Staff have adapted to the video format with dedication and the same passion for their work. Some therapists have found the online setting to be a great fit. Others have found that meeting in person is better for the groups they facilitate.
To guide planning, Seche and Julie Achtyl, program director of Strong Recovery’s outpatient clinic, are asking themselves:
- What is the appropriate balance of in-person and online groups?
- Which group topics fit well with each format?
- How can we support patients with limited technology?
- Which therapists have a particular strength on the video platform?
- How can we align staff strengths with patient needs to improve treatment and access?
Seche sees a bright future for videoconferencing within Strong Recovery’s services: “The positive experience by both patients and clinicians has shifted my thinking about care delivery. Groups as well as individual and family sessions through videoconferencing are added pathways to connecting with our patients.” To ensure these pathways remain open, the program has completed New York State’s certification process to obtain a permanent approval for tele-practice.
To read more about videoconferencing groups and their potential to expand access to care in rural communities, see our main article and our update about their convenience for patients.
References
[1] In addition, a recent article from the Mayo Clinic reviews telehealth interventions for SUD treatment, placing them in the context of the COVID-19 pandemic, and suggests strategies for implementation. Oesterle, T. S., Kolla, B., Risma, C. J., Breitinger, S. A., Rakocevic, D. B., Loukianova, L. L., . . . Gold, M. S. (2020). Substance use disorders and telehealth in the COVID-19 pandemic era. Mayo Clinic Proceedings, 95(12), 2709-2718.
[2] Some patients attended multiple groups. The number of attendees refers to group visits rather than unique visits. July and September totals were affected by the July 4 and Labor Day holidays.